The Role of Infectious Agents in Cancer Development
Viruses and Cancer
Viruses are responsible for an estimated 10% to 15% of human cancers. Several viruses have been identified as cancer-causing agents in humans, including Epstein-Barr virus (EBV), Kaposi sarcoma herpesvirus, hepatitis B virus (HBV), hepatitis C virus (HCV), human T-lymphotropic virus-1 (HTLV-1), human genital papillomavirus, and Merkel cell polyomavirus. These viruses can cause a variety of malignancies, such as Burkitt lymphoma, diffuse large B cell lymphoma, Hodgkin lymphoma, nasopharyngeal carcinoma, gastric adenocarcinoma, leiomyosarcoma, posttransplant lymphoproliferative disease, Kaposi sarcoma, primary effusion lymphoma, multicentric Castleman disease, hepatocellular carcinoma, adult T-cell leukemia, cervical carcinoma, vulvar cancer, anal cancer, head and neck cancers, and Merkel cell carcinoma.
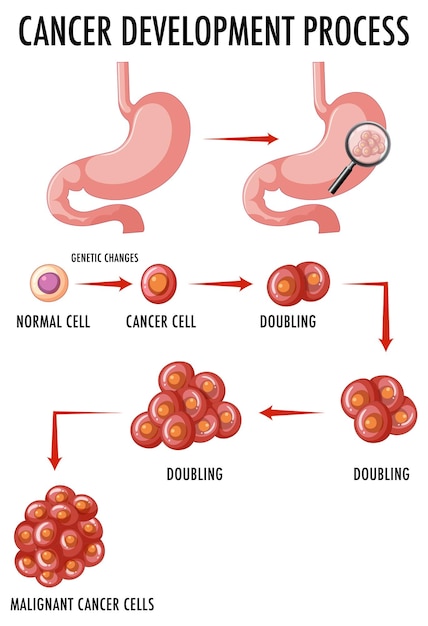
The mechanisms by which viruses cause cancer are still under intense investigation. They can be categorized into two broad categories: direct and indirect causation. Direct causation occurs when viral genes, known as oncogenes, directly influence cellular processes, leading to the development of cancer. Indirect causation, on the other hand, involves chronic inflammation resulting from persistent viral infections, which can create an environment favorable for cancer development. It is important to note that cancer is not the normal outcome of a viral infection but rather an incidental side effect of viral gene products evolved for the normal process of infection or the circumstances of the immune response to infection.
The identification of viruses as the etiological agents of common cancers has paved the way for prevention strategies. Vaccines have been developed for hepatitis B and human papillomavirus, which have been successful in reducing the incidence of liver cancer and cervical cancer, respectively. Furthermore, viruses are being explored as potential oncolytic agents to treat cancer. Their ability to selectively target and kill cancer cells while stimulating an immune response holds promise for future cancer therapies.
Bacteria and Cancer
Bacteria, specifically Helicobacter pylori, were the first microbes to be definitively linked to cancer. H. pylori infection has been associated with an increased risk of stomach cancer. While the association between bacteria and cancer is well-established, the mechanistic basis of this link is still being explored.
Recent research has highlighted the importance of the gastric microbiome and its interaction with H. pylori in the progression of stomach cancer. It has been observed that only a small percentage of individuals infected with H. pylori develop gastric carcinoma or lymphoma, suggesting that other factors, such as strain differences, host differences, and the host’s microbiome, play a role in determining the outcome of H. pylori infection. Changes in the microbiota composition, induced by H. pylori, can further contribute to the development and progression of stomach cancer.
Oral bacteria have also been implicated in the development of oral squamous cell carcinoma, one of the most commonly reported cancers. Porphyromonas and Fusobacterium are two genera of oral bacteria that have been associated with cancer. Specific species within these genera, such as P. gingivalis and F. nucleatum, have been found to modulate intracellular persistence and have immune-disruptive properties. The presence of these bacteria or bacterium-specific antibodies has been correlated with the occurrence of oral squamous cell carcinoma.
The role of bacteria in tumorigenesis extends beyond the oral cavity and stomach. Studies have shown that bacteria, through their interactions with the host microbiota, can influence various aspects of cancer development, including cell proliferation, genome stability, and immune evasion. Although most of the research has focused on gastric and colorectal cancers, recent work has explored the effects of the microbiota on cancer development and progression at other sites in the body.
Aggressive prophylactic antibiotic therapy can perturb the microbiota, leading to potential risks for cancer patients and individuals undergoing hematopoietic stem cell transplants. These perturbations can increase the risk of infection and posttransplant graft-versus-host disease. Strategies to prevent or mitigate the effects of microbiota perturbation are being explored to improve the outcomes of cancer treatments.
Parasites and Cancer
Parasites, particularly single-cell protozoa and multicellular helminths, have also been linked to cancer development. Chronic inflammation induced by parasitic infections can contribute to the formation of cancerous cells. Notable examples include schistosomiasis and malaria, which have been associated with the development of bladder cancer and Burkitt lymphoma, respectively.
Schistosoma-induced malignancies, such as bladder cancer, are a result of chronic inflammation caused by the deposition of parasite eggs in the bladder wall. Similarly, Plasmodium falciparum, the protozoan parasite responsible for malaria, has been shown to up-regulate certain enzymes that induce DNA mutations, leading to the development of Burkitt lymphoma in individuals coinfected with Epstein-Barr virus.
Trichomonas vaginalis, a sexually transmitted protozoan parasite, has recently been associated with an increased risk of prostate cancer. The precise mechanism by which T. vaginalis contributes to prostate cancer development is still under investigation, but it is thought to involve chronic inflammation and the activation of proto-oncogenes.
Several flatworms, such as Schistosoma haematobium, Schistosoma japonicum, Schistosoma mansoni, Opisthorchis viverrini, and Clonorchis sinensis, have also been linked to various types of cancer. The mechanisms of carcinogenesis caused by these parasites are multifactorial and involve the induction of cancer-causing innate immune responses, such as reactive oxygen species and reactive nitrogen species, as well as parasite metabolites that trigger chronic inflammation.
Vaccines targeting the metabolic enzymes of these parasites hold promise for protecting against helminth infections and the cancers they induce. However, the lack of sterilizing immunity and memory response to these parasites presents challenges in developing effective vaccines.
Infectious Agents in Cancer Treatment
Interestingly, infections have not only been associated with cancer development but have also shown potential in cancer treatment strategies. The observation that patients experienced tumor remission when they contracted bacterial infections has led to the exploration of using infections as a part of cancer treatment.
Toxoplasma gondii, a parasite, has demonstrated antineoplastic activity and is being investigated as a potential immunotherapeutic agent. Attenuated mutants of T. gondii have shown promise in stimulating an immune response against tumors. Bacillus Calmette-Guérin (BCG), an attenuated strain of Mycobacterium bovis, is currently the only approved therapy for nonmuscle invasive bladder cancer. It utilizes the immune response triggered by the bacterial infection to combat cancer.
Bacteria, such as Listeria monocytogenes and Salmonella enterica, have been genetically modified to deliver tumor antigens to the immune system, stimulating a cytolytic T lymphocyte response. Viruses, including oncolytic herpes viruses, have also been developed to selectively replicate in tumors and produce immune-stimulating factors. These viruses have shown promise in inducing new immune responses against cancer.
The use of infectious agents as adjuvants or immunotherapeutic agents in cancer therapy is a rapidly evolving field. By harnessing the unique properties of viruses and bacteria, researchers aim to develop innovative and effective treatments for cancer.
Conclusion
Infectious agents play a significant role in the development of cancer. Viruses, bacteria, and parasites have all been linked to various types of malignancies. Understanding the mechanisms by which these infectious agents contribute to cancer development is crucial for developing preventive measures and effective treatments.
Vaccines have already been developed for certain viruses, such as hepatitis B and human papillomavirus, and have shown success in reducing the incidence of associated cancers. Further research is needed to explore the potential of vaccines for other infectious agents linked to cancer.
Meanwhile, the use of infectious agents in cancer treatment is an exciting area of investigation. By utilizing the unique properties of viruses and bacteria, researchers are developing innovative approaches to target and destroy cancer cells while stimulating an immune response against tumors.
As our understanding of the role of infectious agents in cancer continues to grow, we can expect significant advancements in prevention strategies and treatment options. The fight against cancer is multifaceted, and infectious agents are proving to be valuable allies in this battle.